Source: Precision Medical Products
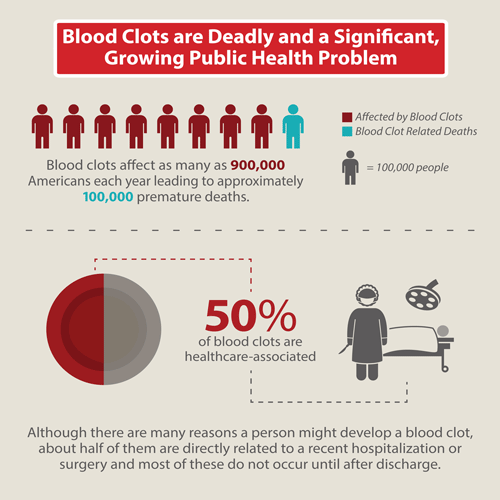
As fast-paced as today’s society has become, people have busy lives and would always prefer treatments and procedures for their medical conditions that can be completed quickly and are not extensively time-consuming. Medical science and technology have evolved accordingly, and the focus is on rapid diagnostic tests, improving patient throughput at hospitals, and ensuring early recovery and mobility. Surgical procedures that once required inpatient admission and long hospital stays can now be performed as ‘day’ procedures. Perhaps, nowhere is this more evident than in orthopedic surgery where many procedures, such as arthroscopy and fracture reduction and fixation, are now routinely performed in outpatient settings. As more and more surgeries are being performed in outpatients, there is a dire need to review practice guidelines with an aim to reducing complications. One of the most significant complications associated with ambulatory surgery is deep vein thrombosis (DVT). The rise in outpatient surgical procedures has coincided with an increase in the incidence of DVT.
Is the risk of DVT after ambulatory surgery underestimated?
Unfortunately, experts believe that ambulatory surgical centres (ASCs) vastly underestimate the individual patient risk of developing a DVT. For one thing, ASCs rarely use a validated assessment tool to document a patient’s risk of developing DVT. The risk level, even if documented correctly, is liable to change during the surgical procedure. Most important, ASCs may not be able to adequately follow up all patients after surgery for DVT development, as this is dependent on patient cooperation communication. DVT in ambulatory orthopedic surgery is not limited to advanced age, or lower limb procedures alone. Any procedure that involves bone manipulation increases the risk of developing DVT.
Guidelines for DVT prophylaxis in ambulatory orthopedic surgery
Notably, existing guidelines for DVT prophylaxis mostly address inpatient procedures, and there is no clear-cut evidence as to what works best with outpatients. While for inpatients, chemical prophylaxis is the norm, this may not work for outpatients as it requires injections, which may not be practical at home. Some ASCs prescribe compression stockings to be worn at home, but their efficacy is questionable. Experts recommend the use of sequential compression devices (SCDs) as the best option for DVT prophylaxis after ambulatory surgery. Traditionally, these were cumbersome devices that were impractical and inconvenient to use. The new generation devices, however, are wireless, battery-operated and lightweight, and can be worn by patients as soon as they return home.
How can ASCs lower the risk of DVT in outpatient procedures?
ASCs need to have a validated risk assessment tool suitable for ambulatory surgery, such as the Caprini risk assessment tool. The risk of the patient must be assessed prior to surgery, and must be updated after the procedure. Very low risk patients do not require prophylaxis. Patients at low risk must use mechanical prophylaxis in the form of sequential compression devices, and moderate and high risk patients must additionally receive anticoagulant (blood thinning) medication.
The biggest challenge to preventing DVT at home is patient compliance. The blood thinning medication, if prescribed, needs to be taken on a daily basis, and the SCD must be worn for at least 18 hours a day. ASCs would benefit from using methods that allow them to monitor patient compliance. The Circul8 device, for instance, has a mobile app that checks whether a patient is following the protocol set by the physician. At follow-up visits, this can be verified, and the patient can be advised accordingly.